Our Work
Here are just a few of the things our interdisciplinary teams have been working on.
Come to our OpenHouse to see all of our current projects.
Naturally occurring retirement communities (NORCs) are regular residential buildings that have become home to a high density of older adults.
The Friendly Neighbour Hotline is a volunteer-driven program to support low-income seniors with food access during the COVID-19 pandemic.
Prescribing Virtual Reality (VRx) is a suite of projects that design and evaluate therapeutic VR-interventions for diverse and challenging populations (patients, caregivers, providers), from community to acute care.
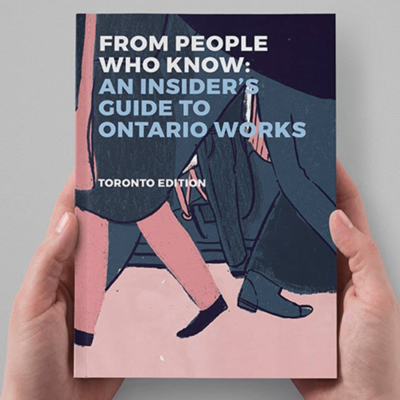
In this series of handbooks, we tap into the expertise of people with lived experience to come up with practical advice, life hacks and ways to gracefully negotiate society’s big institutions.
A simple tool and set of process changes to improve the hospital transition experience for patients codesigned with patients, caregivers, and providers.
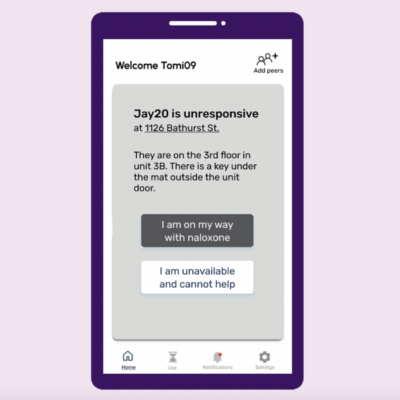
ORN is a mobile app connecting people who use drugs alone with peers who can respond to overdose alerts with naloxone. It takes the concept of a safe consumption site virtual.
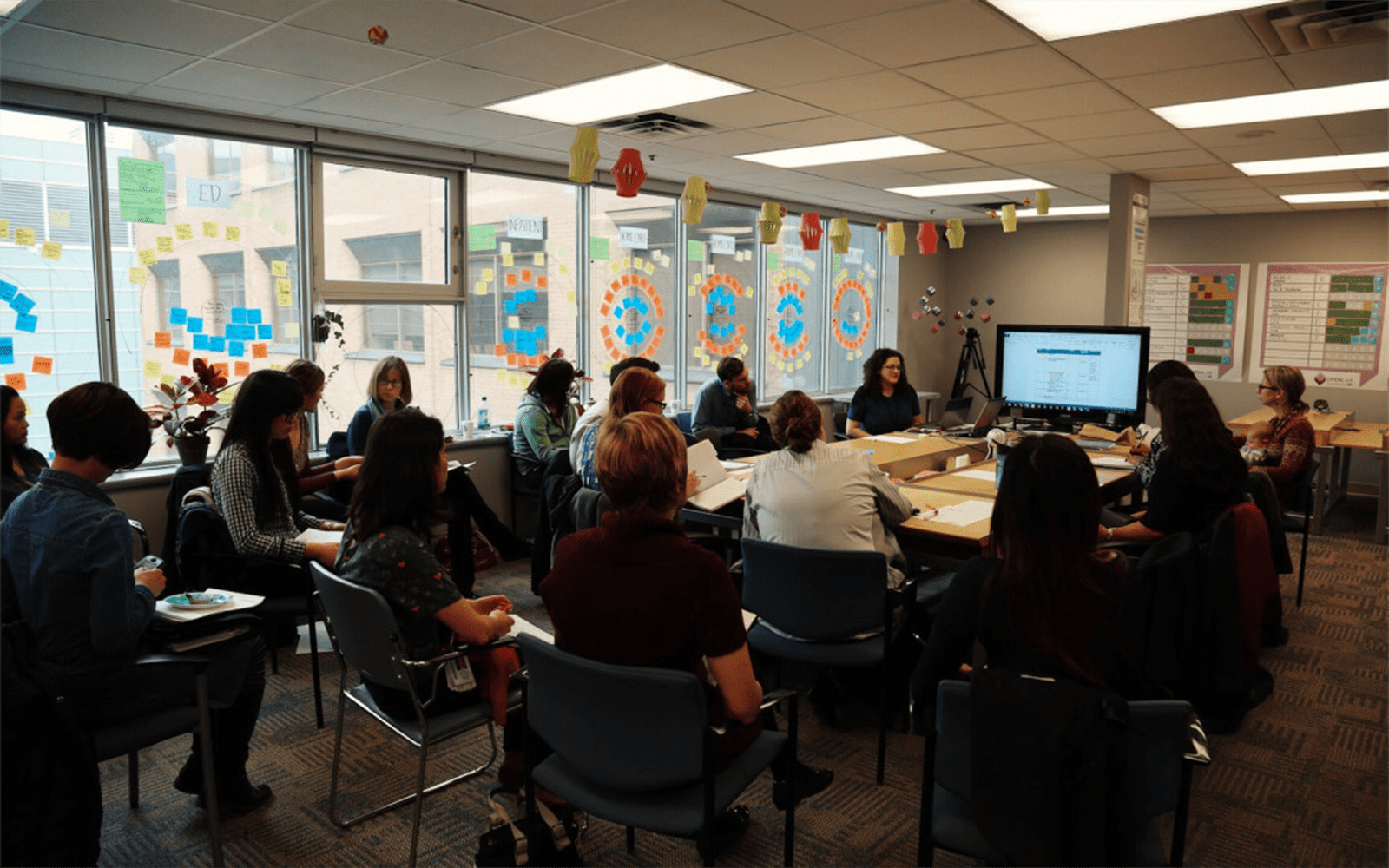
The AFIB Innovation Program redesigns the system and process of care for atrial fibrillation (AFIB) to improve patients' quality of life and the sustainability of the healthcare system from the Emergency room to the Family Doctor's office.
The Local is an award-winning magazine exploring urban health and social issues in Toronto. It began as a hyper-local storytelling project at OpenLab in 2017 and, in 2019, The Local spun off as an independent non-profit.
Have an idea for a project?
With an ever-evolving health system, creative solutions are always needed to improve the way healthcare works. Have a challenge in mind? You don’t have to solve it alone. Let’s talk about your ideas for the next OpenLab project.
Join The Conversation The First Tuesday of Every Month
Curious about our work? Have an idea to contribute? Our monthly gathering is open to anyone who wants to meet our team, learn about current projects, and hear from thought-provoking guest speakers.